

TMJ/ Myofacial
Pain
COMPUTERIZED
DIAGNOSTICS: The Key to Success
"TMJ/TMD" - What Is It?
According to the lay person the TMJ (Temporomandibular Joint) is a term that is often used to identify a multifaceted multi etiologic group of problems that involve both medical as well as dental conditions involving the temporomandibular joint, muscles of mastication, the teeth/occlusion as well as the central nervous system. TMJ is more appropriately called TMD (Temporomandibular Joint Disorder or Dysfunction).
The "TMJ" is a two joint system connected by the main body of the mandible and ramus on each side. The two condyles are the upper boney portion of the jaw bone (mandible) that is housed within the glenoid fossa within the boney skull just forward of the ear (auditory meatus). The condyles are able to swing and rotate within the fossa, but limited by the surround ligamentous attachments (temporomandibular ligaments) and surrounding muscles. The disc (articular disc) is a thin ligamentous tissue that acts like a cushion between the condylar head and upper glenoid fossa of the skull. Attached to the articular disc are fine muscles (lateral pterygoids) as well as surrounding ligaments that help in positioning the disc over the condyles as they move within the joint compartment during functioning and resting modes.
The temporomandibular joints are the only two joints that function together as a single unit unlike any other joint in the body in that they must coordinate with the coming together of the upper and lower teeth (accompanied by the surrounding periodontal ligamentous attachments, nerves and surrounding bones and gum tissue, during opening and closing cycles of chewing, swallowing, breathing, talking, wistling, kissing, sucking and resting modes.
Common problems that can occur with the temporomandibular joint are disc disorders or internal derangments of the disc, disc locations, tearing of the lateral and medial collateral ligaments due to traumatic injuries, inflammatory disorders as synovitis/capsulities, inflammatory arthritis, capsular fibrosis, ankyosis, subluxations, spontaneous dislocations, chronic (recurrent disclocations) contributing to clicks and audible popping sounds. Fractures and hemarthrosis within the TM Joint should also be considered. Masticatory disorders (muscle pain), chronic mandibular hypomobility, mandibular hypermobility, growth disorders of the jaw (i.e. coronoid hyperplasia), and functional abnormal jaw closure patterns also be recognized. Common misdiagnosis' are fibromyalgia, migraineous head pain, neuralgias of the masticatory system as well as cervical/neck/ shoulder and back pain.
What Is Your Perspective?
Various experts have tried to identify this problem with various names such as: "TMJ", Craniomandibular Dysfunction (CMD), Temporomandibular Joint Dysfunction (TMD), Myofacial Pain Dysfunction (MPD), Cranio-facial Dysfunction (CFD), and Musculoskeletal Dysfunction. Depending on which philosophical belief and school of thought dental experts and clinicians believe that it relates to a lack of coordination between the muscles of mastication, the jaw joints, the teeth and the central nervous system. Academics may also call it Cranio-mandibular/ Neurovasomuscular/Cervical Dysfunction. Third party insurance groups may recognize it as, Musculoskeletal Dysfunction (MSD) of the head and neck resulting in Temporomandibular Joint Dysfunction.
An Awareness of the Numerous Signs and
Symptoms of TMJ
Today, our dental professions diagnostic paradigms are evolving beyond only identification of dental caries, marginal breakdown of old fillings and crowns, root canal lesions, fractured teeth and periodontal breakdown. These basic dental problems are often only indications of a more hidden muscular, occlusal and temporomandibular joint problem that go often undetected, even within the medical and dental profession. TMJ/TMD is a problem that is not easily seen by cursory dental x-ray and intra-oral evaluation. It presents with many signs and symptoms that can mimic other medical and dental problems as vascular disorders, brain tumors, aneurisms, cervical disc disorders, throat and oral cancer, etc.
Some of the numerous signs and symptoms may include clicking, popping and grating noises of the jaw joints. Consider the tender paining temporal muscles on the side of the head. Tender and sore muscles behind the head and neck (sub-occipital cervical region) as well as upper shoulders can be part of this problem. Muscles under the chin, the facial muscles (side of face), limited mouth opening, loose teeth, clenching/ bruxing, postural problems, paresthesia of fingertips and hands, nervousness, insomnia are just a few of the over 12o different signs and symptoms of TMJ. What about those cases with non-specific facial pain, tenderness on palpation of various sites of the head and neck? Teeth sensitivities and aches, ear congestion feelings, pain behind the eyes, tingling in the arms and fingers, dizziness, ringing in the ears, etc., all relate to the dental aspect of TMJ. Many of these symptoms are related to and are associated with the living tissues that effect the mandibular position and in turn effect upper to lower teeth relationships and vice versa.
Crowded lower anterior teeth, wear of the lower incisal edges, fractured cusps, narrow arches, vaulted palates, deep curves of Spee, over-closed bites, flared upper anterior teeth, locked upper buccal cusps, facets, cervical erosion (abfractions), receding gums, mobile teeth, open interproximal contacts, loss of molars, cross bites, anterior open bites, anterior tongue thrust, lateral tongue thrust, midline discrepancy, to name some of the intra-oral signs.
Extra-oral signs as: facial asymmetry bilaterally, short lower third of the face (chin to nose point diminished), chelitis, abnormal lip posture, deep mental crease on chin, dished-out or flat labial profile, facial edema, mandibular torticollis, cervical toricollis, forward head posture (lordosis) elongated lower face (steep mandibular angle), and speech abnormalities, should all be considered as abnormal signs. The human body, which includes the teeth, the muscles of the head and neck, the TM Joints, the neurology that innervates the system of mastication and posturing of the head and neck are all parts of what the dental profession should consider when diagnosing and treating our patients comprehensively.
If you are experiencing such and are not getting better you are not alone. These type of symptoms are signs of temporomandibular joint dysfunction (TMJ) which are a common problem among 10 million people in the USA. Approximately 1 in 27 or 3.68% of all people in USA experience these types of symptoms daily (National Insititute for Dental and Craniofacial Research). Many TMJ patients have received numerous listed medical and dental treatments with little to no effective relief of their pain. Many of the treatments have been recommended based on the doctors preference and not based on sound objective measured scientific evidence for both saftey and effectiveness. Some treatments have been tried, some invasive, irreversible, and made the patient worse, leaving the patient in a dilemma of financial loss, disappointment, depression and dispare.
SYMPTOMS
The symptoms most commonly cited are as follows:
- Facial pain
- Jaw joint pain
- Back, Neck, cervical pain
- Postural problems (forward head posture)
- Pain in the face
- Limited opening of the mouth
- Headaches (tension type)
- Pain in the muscles surrounding the temporomandibular joints
- Pain in the occipital (back), temporal (side), frontal (front), or sub-orbital (below the eyes)
- Pain behind the eyes - dagger and ice pick feelings
- Multiple bites that feels uncomfortable or, "off," and continually changing
- Clenching/bruxing
- Tender sensitive teeth to cold
- Deviation of the jaw to one side
- The jaw locking open or closed
- Ringing in the ears, ear pain, and ear congestion feelings
- Sinus like symptoms
- Dizziness or vertigo
- Visual Disturbances
- Tingling in fingers and hands
- Insomnia - difficulty sleeping
This list of subjective symptoms is by no means exhaustive, but does provide a
good idea of the nature of the complaints that are often made by those suffering
from TMD.
Diagnostic Classification Confusion
The NIH Technology Assessment Conference Statement concluded that, "there are
significant problems with present diagnostic classifications of TMD, because
these classifications appear to be based on signs and symptoms rather than on
etiology." They further state that, "...scientifically based
guidelines for diagnosis ... are still unavailable."
The medical and dental community usually diagnoses TMJ based on
range of motion tests, listening for sounds in the joints, examining the teeth,
and manual palpation of the jaw joints as well as the muscles of the face, and head. Typically the dentist may ask for information about your pain and other
symptoms, injuries, oral habits, and previous medical and dental treatments. A subjective assessment and examination may be completed, but often without confirmation of objective measured instrumentation and analysis, which is now becoming a standard with the community scientific methodology and standards and those clinicians who are seeking a higher standard of objective care for their patients.
EDUCATING YOURSELF ABOUT TMJ
The following are recommended guidlines from "The TMJ Association, Ltd", a patient based advocacy organization:
Consult Your Medical
Doctor
We recommend that you first consult with a medical doctor to rule out any
disease that may be causing your symptoms and is treated by medical
practitioners. If they are unable to find a reason for your problem, and you are
referred to a dentist for a TMJ evaluation, we encourage you to then obtain
multiple INDEPENDENT opinions on your condition.
Get an Independent Opinion
To be a truly independent opinion, the medical/dental professional can not be
associated with or working with the medical/dental professional from whom you
have already received an opinion. Many TMJ patients seek further opinions
outside of their geographical area, without the referral of their original
medical/dental professional.
Educate Yourself and
Others
With the increase of managed care (HMOs), where a primary care physician is your
health care gatekeeper it is mandatory that you, the patient, become your own
well-informed advocate. You will also need to educate your primary care
physician and all others you encounter within the system about TMJ.
Musculoskeletal
Dysfunction (MSD) of the Head and Neck Resulting in
Temporomandibular (Jaw) Joint Dysfunction ("TMJ")
(Some portions of the following section contains excerpts of writings from Dr. James Garry, who is an expert in treating musculoskeletal dysfunctions of the head, neck and temporomandibular joint dysfunction as well as air-way obstruction/ sleep apnea problems).
Patients suffering facial pain, headaches, neck
aches, shoulder, and/ or back pain often have to learn to live with the pain.
Some patients have subjective hearing loss, ringing of the ears, dizziness, pain
in the ear, a feeling of fullness or pressure in the ears, clicking/ popping of
the jaw joints and eye pain. The mouth, teeth and throat may also be affected. When
competent clinicians cannot find an organic basis for these symptoms, they often
suggest it might be psychogenic.
There is a classification of disease known as Musculoskeletal Dysfunction of
the head and neck (MSD). MSD seems totally unrelated to symptoms such as
back pain or ear disorders. Yet, correction of this condition may alleviate many
medical symptoms; acute or chronic diseases of the ear, nose, throat, head,
neck, shoulder and back. The syndrome is medically as well as dentally
related.
TMJ/ MSD is a dysfunction of a group of associated muscles, ligaments, nerves
and supportive structures that are associated with the temporomandibular joint.
Unfortunately, TMJ/ TMD is one of the most misdiagnosed of the medical/ dental
conditions. There are two aspects that contributes to this sad phenomenon of
misdiagnosis.
First, few doctors including physicians, ENT specialists, dentists,
chiropractors, osteopaths, etc. have a comprehensive understanding and
perspective in the diagnosis and treatment of TMJ/ MSD.
Secondly, these disorders have many overlapping symptoms which mimic many other
conditions such as neurological disorders, ringing and fullness in the ear,
headaches, etc.
Misdiagnosis is the rule rather than the exception with MSD. Patients
wander from specialist to specialist, depending on the type of pain and problems
they experience. Symptoms focusing on ear, sinuses, or swallowing problems are
referred to the Otolaryngologist. Limitations of jaw movement are referred to
the Orthopedist. Persistent head pains are referred to the Neurologist, etc.
As the wanderers are told and retold that there seems to be no organic basis for
their pain, that the cause is psychogenic, their anxiety mounts. When physical
findings remain obstinately in abeyance, patients may begin to suspect a brain
tumor, turn to drugs to alleviate their symptoms, or on rare occasions, even
contemplate suicide.
ANATOMY OF TEMPOROMANDIBULAR JOINT:
The Temporomandibular Joint is the joint connecting the jaw (mandible) to the
skull (temporal bone).
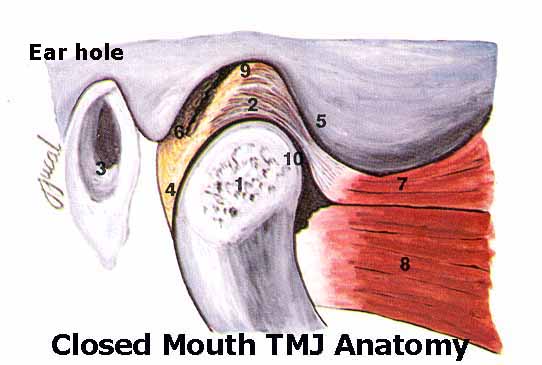 The two bones are held together and function via a complex group of muscles,
ligaments and other soft tissue. The temporal bone has a concavity call the
glenoid fossa in which the head of the jawbone (the condyle)sits. A cartilage
disc call the articular disc separates the two bones. The articular disc slides
in conjunction with the mandible to provide smooth quiet movement and acts as a
cushion against heavy forces generated by the strong jaw muscles. The right and
left TMJ joints do not act as a separate joints, but must move in coordination
with one another.
The two bones are held together and function via a complex group of muscles,
ligaments and other soft tissue. The temporal bone has a concavity call the
glenoid fossa in which the head of the jawbone (the condyle)sits. A cartilage
disc call the articular disc separates the two bones. The articular disc slides
in conjunction with the mandible to provide smooth quiet movement and acts as a
cushion against heavy forces generated by the strong jaw muscles. The right and
left TMJ joints do not act as a separate joints, but must move in coordination
with one another.
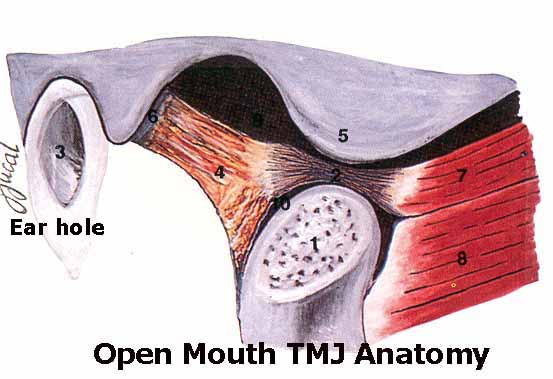 The TMJ joints are considered the most complex joints in the human body because
they must provide for rotational movements, sliding movements and an infinite
range of combined movements and functions, unlike any other joint in the body.
The TMJ joints are considered the most complex joints in the human body because
they must provide for rotational movements, sliding movements and an infinite
range of combined movements and functions, unlike any other joint in the body.
The lower jaw (Mandible) has a relationship to the upper jaw (Maxilla). If
this relationship is altered, the muscles of mastication (chewing muscles) go
into spasm. This causes the muscles that have the same nerve intervention to
also go into spasm. The resulting stresses may radiate throughout the head,
neck, and even involve the back. The pain may be constant or intermittent,
lasting minutes, hours, days, or even years. Many patients describe the pain as
a migraine headache. Eventually a patient may demonstrate clicking, grating,
snapping, or popping sounds in the joint.
MECHANICS OF TEMPOROMANDIBULAR JOINT DYSFUNCTION:
The lower jaw may be over closed (too close to the upper jaw), and /or distally
displaced (too far back in the joint or socket). Also, the lower jaw may deviate
to one side due to interfering tooth cusps (points on the chewing surfaces of
teeth that do not meet properly with the opposing teeth).
The cause is multifaceted, i.e., loss of teeth, poor alignment or natural
wear of teeth, grinding or clenching of the teeth day and night, poor tongue
position, a muscle imbalance in the tongue and the facial muscles, chronic mouth
breathing, osteoarthritis, rheumatoid arthritis, trauma, etc.
To determine if an improper relationship exists between upper arch and the lower
jaw, it is necessary to relax the muscles of mastication (chewing muscles), then
close the relaxed lower jaw on a trajectory that is not strained. In other
words, the mouth closes where the muscles are most comfortable.
To relax the muscles of mastication, a gentle pulsating stimulus is applied to
the skin for approximately one hours. Multi-channel electromyography (EMG) is
used to verify the degree of muscular relaxation.
MSD is not a rare condition. Every patient has some degree of Musculoskeletal
dysfunction. It is when symptoms are manifested that people seek help. Many
patients tend to clench and/or grind their teeth in response to unconscious
stress, creating muscular dysfunction. This usually occurs during sleep, but it
may also occur during a stressful daily experience. Resolution of unconscious
stress which cause symptoms indicated on the Screening questionnaire may require
stress counseling. Subconscious stress must be controlled for successful
resolution of clenching and /or grinding of teeth.
POSTURE AND AIRWAY
Posture has an effect on the relationship of the lower jaw to the cranium and
can result in a malocclusion (improper bite). If body symmetry is not within
normal limits, physical therapy may be necessary to correct body symmetry during
treatment.



Airway obstruction must be cleared as it will result in constant mouth breathing. Allergy is a primary cause of chronic mouth breathing. If nasal obstruction is evident, consultation with an allergist and/or Otolaryngologist will be recommended during treatment. All chronic mouth breathers develop an improper bite (malocclusion).
INITIAL TREATMENT FOR TMJ:
Three approaches or a combination thereof, may be recommended as initial therapy:
1. Occlusal correction or coronoplasty (reshaping teeth to remove interferences that cause abnormal jaw displacement).
2. Construct an orthotic to orthopedically align the lower jaw to the cranium in three dimensions providing there is an over closure. If symptoms subside after wearing the appliance for three months, crowns may be recommended to maintain the orthopedic position established by the orthotic. Orthododontia may be recommended to avoid crowns. Possibly a combination of orthodontia and crowns will be recommended. When posterior (back) teeth are missing, dentures and /or partials may be recommended. For more details, see OUR TREATMENT PROTOCOL
3. Surgery is the last and least recommended when irreversible damage has occurred in the joints and is beyond natures healing capacity.